Anatomy & Histology & Function
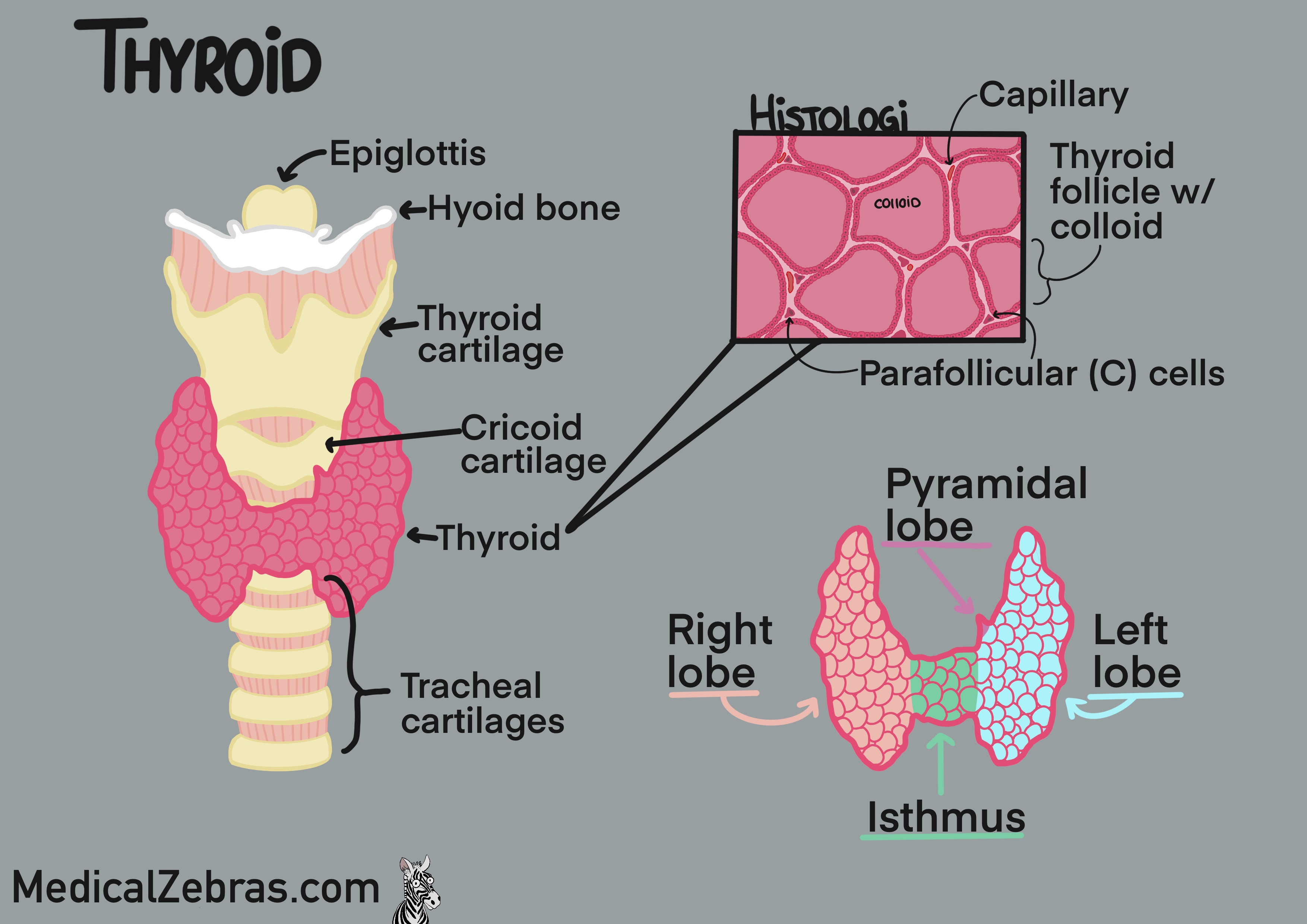
The thyroid gland is a butterfly-shaped gland located in the front of
the neck, just below the larynx. It consists of two lobes, one
on each side of the trachea, connected by a thin piece of tissue
called the isthmus. As the thyroid gland is formed it moves
from the base of the tongue to its final position in the neck via the
thyroglossal duct. Because of this migration, the thyroid gland can
sometimes be found in other locations, such as higher up in the neck
or even in the chest, known as an ectopic thyroid gland. Most often
you end up with a small strip of thyroid gland extending superiorily
from the isthmus or one of the lobes called the pyramidal lobe.
Histologically the thyroid gland is made up of spherical structures called follicles, which are lined with a single layer of epithelial cells called follicular cells. The follicles are filled with a substance called colloid, which contains the precursor to thyroid hormones. (T3 and T4). Surrounding the follicles are parafollicular cells (also known as C-cells), which produce the hormone calcitonin. Between the follicles are connective tissue and blood vessels allowing for efficient transport of hormones.
Histology:
Histologically the thyroid gland is made up of spherical structures called follicles, which are lined with a single layer of epithelial cells called follicular cells. The follicles are filled with a substance called colloid, which contains the precursor to thyroid hormones. (T3 and T4). Surrounding the follicles are parafollicular cells (also known as C-cells), which produce the hormone calcitonin. Between the follicles are connective tissue and blood vessels allowing for efficient transport of hormones.
Histology:
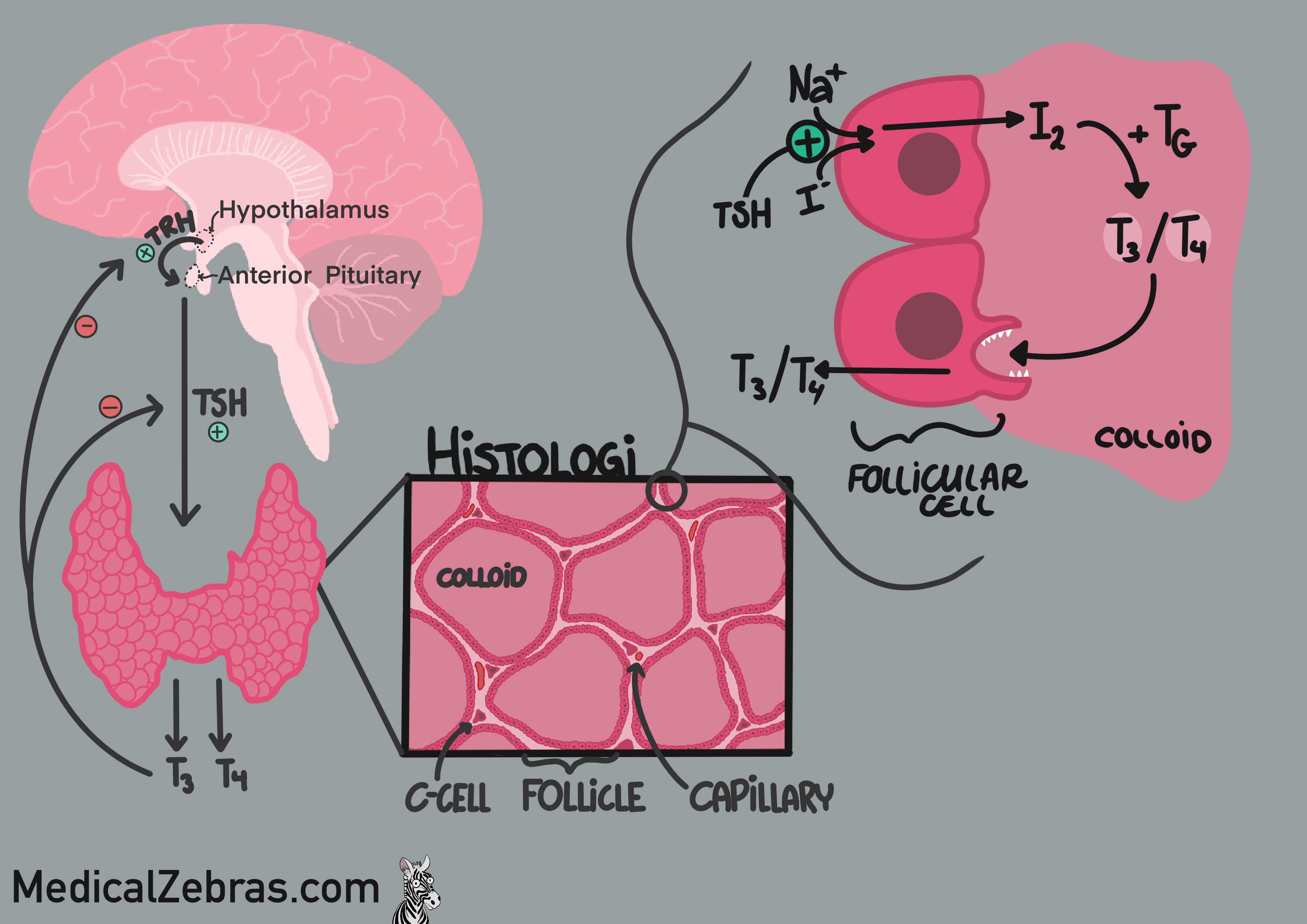
- Follicular cells (epithelial cells) take up iodine and release it into the colloid where it is used to make precursers of T3 and T4. Which is then taken up by the follicular cells, again, cleaved by proteases, and released into the blood stream as T3 and T4.
- Colloid contains thyroglobulin, a protein that is used to make thyroid hormones.
- Parafollicular cells (C-cells) produce the hormone calcitonin, which inhibits osteoclast activity (cells that break down bone and release calcium into the blood), and also promote the excretion of calcium and phosphate in the kidneys. This results in a decrease in blood calcium levels.
How to activate the thyroid gland: The journey start in the
hypothalamus where the thyroid receptor hormone (TRH) is secreted.
This hormone than stimulates the anterior pituitary gland to secrete
thyroid stimulating hormone (TSH). TSH travels to the thyroid where it
connects to a transporter on the outer side of the follicular cells,
which then activates a channel called the sodium-iodide symporter
(NIS). This channel then takes up iodine and along with natrium
transports it from the blood into the follicular cell. The iodine is
oxidized within the cell and transferred into the lumen of the
follicle or the colloid. Here the iodine is combined to tyrosine
inside a protein called thyroidglobulin, becoming MIP and DIP. MIP and
DIP are then combined to form T3 and T4, which are still bound to the
thyroglobulin. When the body needs thyroid hormones, the follicular
cells endocytose some of the colloid containing the thyroglobulin with
T3 and T4 attached. The vesicle containing the colloid fuses with a
lysosome, where proteases cleave T3 and T4 from the thyroglobulin. The
free T3 and T4 are then released into the bloodstream. In the blood,
most of T3 and T4 are bound to carrier proteins, such as
thyroxine-binding globulin (TBG), transthyretin, and albumin. Only a
small fraction of T3 and T4 are free and biologically active. T4 is
converted to the more active T3 in peripheral tissues by the enzyme
deiodinase. T3 then enters cells and binds to thyroid hormone
receptors in the nucleus, where it regulates gene expression and
affects metabolism, growth, and development.
Diagnostic methods
Blood test
To test how the thyroids function, most often "TSH", "T3" and "T4" are checked.Imaging
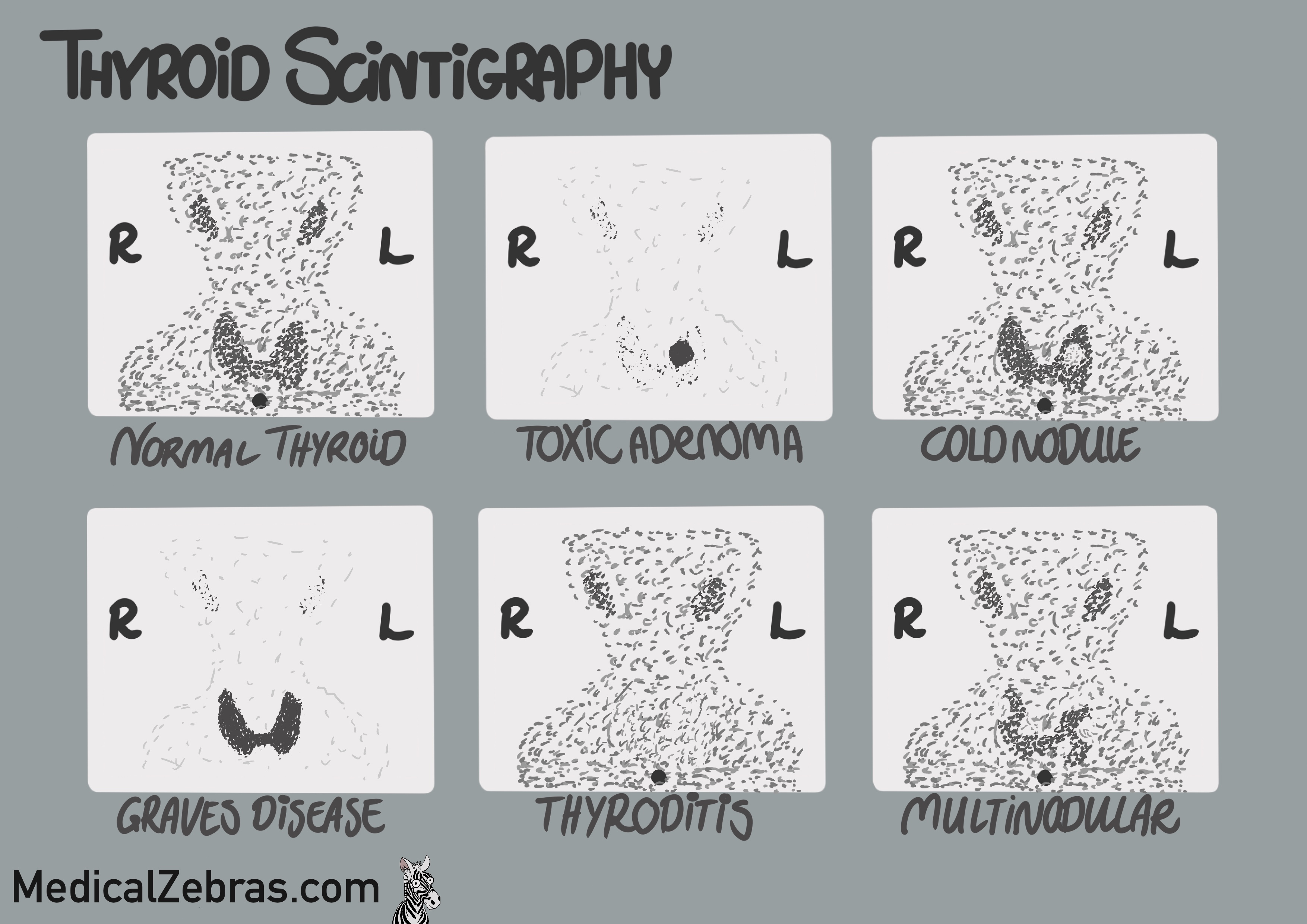
Thyroid Scintigraphy
Thyroid scintigraphy is a nuclear imaging technique that uses small amounts of radioactive material to evaluate the function and structure of the thyroid gland. The patient is injected with a small amount of radioactive iodine or technetium, which is taken up by the thyroid gland. A special camera, collimator, is used to detect and gather the radiation emitted by the radioactive material, and you are able to visualise the gland. As the radioactive material is also taken up by the salivary glands, most often they can be visualised as well.Pros:
- Great way to easily assess the thyroid tissue function
- Cannot detect lesions under 1 cm.
- Cannot detect cold/hypofunctioning lesions if there is normal thyroid tissue infront or behind (here a SPECT/CT would be preferred, as you can then inspect the uptake in 3D).
- Radioactive material is used.
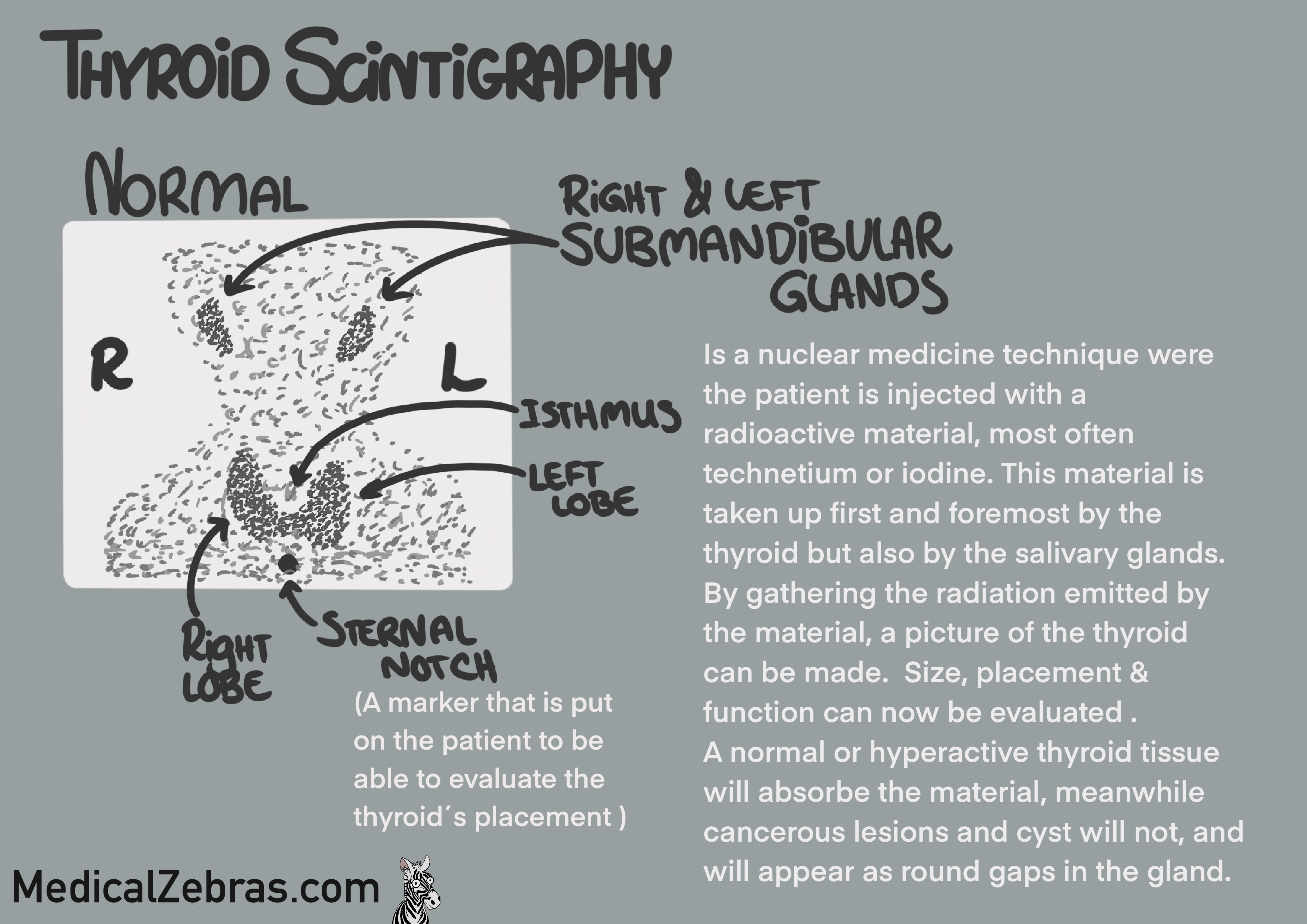
Interpretation
- Normal scan: Uniform uptake of the radioactive material throughout the thyroid gland, indicating normal function. You will also see uptake in the salivary glands.
- Hyperactive thyroid or nodule (hot/toxic nodule): Increased uptake of the radioactive material throughout the thyroid or in a specific area, indicating hyperfunctioning tissue. Simulatiously, there will be decreased uptake in the salivary glands and also the rest of the thyroid gland (if it is a nodule) as the hyperfunctioning tissue is taking up most of the radioactive material.
- Hypoactive thyroid nodule (cold nodule): Decreased uptake of the radioactive material in a specific area of the thyroid gland, indicating hypofunctioning tissue. As there is a small risk of a hypoactive nodule being malignant, further investigation with ultrasound is needed to evaluate the structure of the nodule, to further evaluate the risk of malignancy and the need for a biopsy. But this can also be due to benign causes such as cysts or colloid nodules.
- Multinodular goiter: Multiple areas of increased and decreased uptake of the radioactive material throughout the thyroid gland, indicating the presence of multiple nodules with varying levels of function.
- Diffuse decreased uptake of the radioactive material throughout the thyroid gland, and normal uptake in the salivary glands. Could indicate inflammation (thyroiditis) or be caused by iodine-induced hypothyroidism, or the presence of medications that interfere with iodine uptake (such as amiodarone or lithium, or levothyroxine (decreases TSH)) or iodine-containing contrast agents (used for CT-scans) that compete for thyroid uptake.
-
Artifacts:
- Uptake in the esophagus or stomach if the patient has swallowed some of the radioactive material, that has been secreted into the saliva and then swallowed. Drinking water before the scan can help reduce this artifact.
- High levels of circulating thyroid hormones, which can suppress the uptake of the radioactive material. This can be seen in patients with hyperthyroidism or thyroiditis.
Ultrasound
Ultrasound is most often used to evaluate the size and shape of the
thyroid, if there is a risk of malignant nodules in the thyroid or
if there are cysts that can be drained.
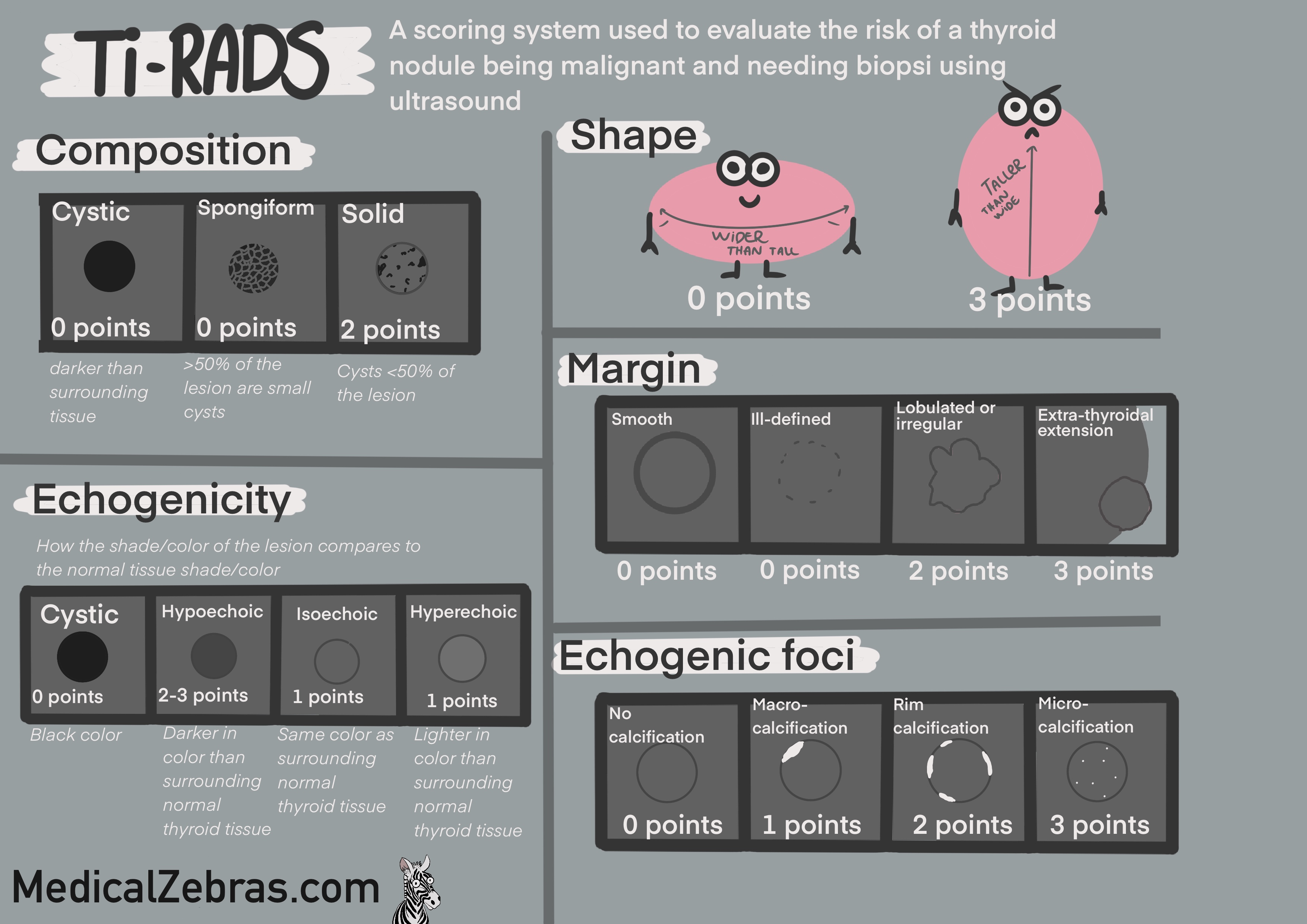
All nodules are classified according to the ACR TI-RADS system (American College of Radiology Thyroid Imaging, Reporting and Data System). This system uses a point system to classify the nodules from TR1-TR5, where TR1 is benign and TR5 is highly suspicious of malignancy. The points are given based on the following criteria:
Pros:
All nodules are classified according to the ACR TI-RADS system (American College of Radiology Thyroid Imaging, Reporting and Data System). This system uses a point system to classify the nodules from TR1-TR5, where TR1 is benign and TR5 is highly suspicious of malignancy. The points are given based on the following criteria:
-
Composition
-
cystic (0)
-
spongiform (0)
-
mixed cystic and solid (1)
-
solid or almost completely solid(2)
-
Echogenicity
-
anechoic (0)
-
hyperechoic or isoechoic (1)
-
hypoechoic (2)
-
very hypoechoic(3)
-
Shape
-
wider-than-tall (0)
-
taller-than-wide (3)
-
Margin
-
smooth (0)
-
ill-defined(0)
-
lobulated or irregular (2)
-
extra-thyroidal extension (3)
-
Echogenic foci
-
none or large comet-tail artifacts (0)
-
macrocalcifications (1)
-
peripheral (rim) calcifications (2)
-
punctate echogenic foci (3)
- TR1 (0 points): Benign => No FNA needed
- TR2 (2 points): Not suspicious => No FNA needed
- TR3 (3 points): Mildly suspicious => FNA if nodule is ≥2.5 cm
- TR4 (4-6 points): Moderately suspicious => FNA if nodule is ≥1.5 cm
- TR5 (7 or more points): Highly suspicious => FNA if nodule is ≥1.0 cm
Pros:
- Great way to easily assess the thyroid tissue structure
- User dependent.
- Might lead to over-diagnosis of small benign nodules, leading to overuse of unnecessary biopsies.